Complex bite problems may require jaw surgery in conjunction with orthodontic treatment.
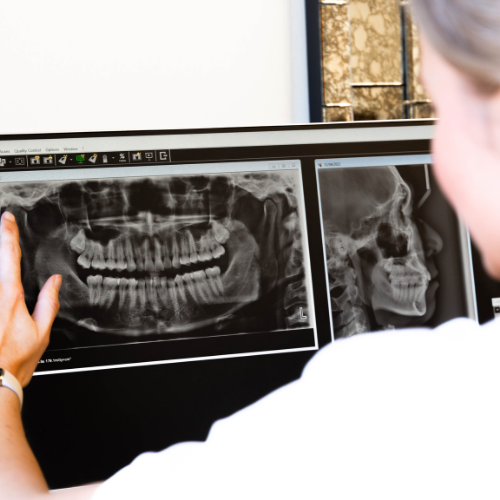
When is jaw surgery needed?
Some people are born with skeletal irregularities that prevent a normal bite, resulting in underbite, overbite, or an open bite. These issues — also called severe malocclusion — can lead to difficulties with chewing (which may affect digestion), speech problems, headaches, jaw joint discomfort, and changes to facial appearance, particularly the profile. Depending on the severity, a bad bite can be corrected with orthodontic treatment or, in more complex cases, jaw surgery.
Jaw surgery (orthognathic surgery) is required in adolescents or adults when the skeletal discrepancy is too significant for orthodontic treatment alone. In adolescents with growth-related bite issues, surgery may be performed before age 18; otherwise, it is generally considered after the growth spurt or in adulthood.
If you are concerned about your child’s bite, consult your dentist — even if they have not yet developed all their permanent teeth — as bone growth and tooth eruption occur independently. With timely intervention, many adolescents can avoid surgery through modern orthodontic guidance during growth. In pre-adolescent children, growth modification is the preferred treatment option, except in cases of congenital deformities or trauma-related conditions.
The Jaw Surgery Process
Pre-surgical orthodontics
The surgical procedure
Post-surgical planning and care
Frequently Asked Questions
How long does recovery take after jaw surgery?
Recovery varies depending on the complexity of your procedure. Most patients can expect initial healing within a few weeks, but full recovery and final results may take several months. Your surgeon will provide a detailed timeline based on your individual case.
When will I be able to eat solid foods after jaw surgery?
Will I need to stay in the hospital?
Some procedures are done on an outpatient basis, while others require hospital admission. If hospital admission is needed, you will typically be admitted on the morning of surgery. Your surgeon will discuss this with you in advance.
Will I experience discomfort after jaw surgery?
Some discomfort is normal, especially in the first few days. Your surgeon will recommend appropriate pain management strategies, including medications and care instructions to help you stay comfortable during recovery.
Will I have trouble talking after jaw surgery?
You should expect some soreness in lengthy conversations; however, the more you talk, the more you exercise your weakened muscles and hence speed recovery.
How much pain will I experience during jaw surgery?
The level of pain experienced after jaw surgery varies from individual to individual. Some patients describe it as more like a “soreness” but most patients call it “discomfort”.
Will there be visible scars?
No. All incisions are made inside the mouth, usually hidden in tissue folds. Sutures either dissolve on their own or are removed after five to seven days.
Can orthodontics alone correct my bite?
In many adolescents, modern orthodontics can guide jaw growth and may prevent the need for surgery. However, surgery is required when the deformity is too severe to be corrected with braces alone.
Who will perform my jaw surgery?
At Smile Solutions, our Oral and Maxillofacial Surgeons are registered specialists with the Dental Board of Australia and the Royal Australasian College of Dental Surgeons after successfully completing their final specialty examinations (FRACDS).
Oral & maxillofacial surgeons undergo 15 to 17 years of continuous study, earning degrees in both Dentistry and Medicine, followed by an additional four years of specialist training in oral & maxillofacial surgery. Depending on their area of interest, they may also hold a Master’s degree, such as in Paediatric Maxillofacial Surgery or Surgical Anatomy.
A/Prof. Patrishia Bordbar
Specialist Oral & Cranio-Maxillofacial Surgeon
B.D.Sc. (Melb.), M.B.B.S (Hons.) (Melb.), PGDip.Surg.Anat (Melb.), M.D.Sc (O.M.S.)(Melb.), F.R.A.C.D.S (O.M.S.), F.R.C.S (Ed.)
Dr Ricky Kumar
Specialist Oral & Maxillofacial Surgeon
BHB (Auck), MBChB (Auck), BDS (Otago), FRACDS (OMS)

Contact Us
Contact Us
"*" indicates required fields